Category Archive 'Medicine'
03 Jun 2021

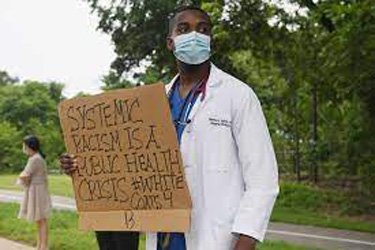
Bari Weiss finds that a number of doctors are speaking out about the problem.
I’ve heard from doctors who’ve been reported to their departments for criticizing residents for being late. (It was seen by their trainees as an act of racism.) I’ve heard from doctors who’ve stopped giving trainees honest feedback for fear of retaliation. I’ve spoken to those who have seen clinicians and residents refuse to treat patients based on their race or their perceived conservative politics.
Some of these doctors say that there is a “purge” underway in the world of American medicine: question the current orthodoxy and you will be pushed out. They are so worried about the dangers of speaking out about their concerns that they will not let me identify them except by the region of the country where they work.
“People are afraid to speak honestly,” said a doctor who immigrated to the U.S. from the Soviet Union. “It’s like back to the USSR, where you could only speak to the ones you trust.” If the authorities found out, you could lose your job, your status, you could go to jail or worse. The fear here is not dissimilar.
When doctors do speak out, shared another, “the reaction is savage. And you better be tenured and you better have very thick skin.”
“We’re afraid of what’s happening to other people happening to us,” a doctor on the West Coast told me. “We are seeing people being fired. We are seeing people’s reputations being sullied. There are members of our group who say, ‘I will be asked to leave a board. I will endanger the work of the nonprofit that I lead if this comes out.’ People are at risk of being totally marginalized and having to leave their institutions.”
While the hyper focus on identity is seen by many proponents of social justice ideology as a necessary corrective to America’s past sins, some people working in medicine are deeply concerned by what “justice” and “equity” actually look like in practice.
“The intellectual foundation for this movement is the Marxist view of the world, but stripped of economics and replaced with race determinism,” one psychologist explained. “Because you have a huge group of people, mostly people of color, who have been underserved, it was inevitable that this model was going to be applied to the world of medicine. And it has been.”
“Wokeness feels like an existential threat,” a doctor from the Northwest said. “In health care, innovation depends on open, objective inquiry into complex problems, but that’s now undermined by this simplistic and racialized worldview where racism is seen as the cause of all disparities, despite robust data showing it’s not that simple.”
“Whole research areas are off-limits,” he said, adding that some of what is being published in the nation’s top journals is “shoddy as hell.”
RTWT
———————-
And here’s an example of what she’s talking about:
The editor-in-chief of the prestigious medical journal JAMA will step down June 30 following backlash after an editor at the publication made controversial comments about racism in medicine, the Chicago-based American Medical Association (AMA) announced Tuesday.
Dr. Howard Bauchner has been editor-in-chief of JAMA and JAMA Network since 2011, but he’s been on administrative leave since March when comments about structural racism made by another editor on the publication’s podcast, and a tweet promoting the podcast, sparked outrage.
“I remain profoundly disappointed in myself for the lapses that led to the publishing of the tweet and podcast,” Dr. Bauchner said in the announcement. “Although I did not write or even see the tweet, or create the podcast, as editor-in-chief, I am ultimately responsible for them.”
Dr. Edward Livingston, a deputy editor at JAMA — who is white — said structural racism no longer existed in the U.S. during a Feb. 24 podcast, The New York Times reported.
“Structural racism is an unfortunate term,” Dr. Livingston, said during the podcast, according to The Times. “Personally, I think taking racism out of the conversation will help. Many people like myself are offended by the implication that we are somehow racist.”
In a now-deleted tweet promoting the podcast, The New York Times said the journal wrote, “No physician is racist, so how can there be structural racism in health care?”
Livingston later resigned, the Times reported.
Over 9,000 individuals have signed a change.org petition following the podcast and accompanying tweet calling for a review of Bauchner’s leadership as well as changes in the editorial process to ensure a more inclusive publication.
“The podcast and associated promotional message are extremely problematic for minoritized members of our medical community,” the petition, created by the Institute for Antiracism in Medicine, says. “Racism was created with intention and must therefore be undone with intention. Structural racism has deeply permeated the field of medicine and must be actively dissolved through proper antiracist education and purposeful equitable policy creation.”
In place of the now-deleted podcast is an apology from Bauchner.
“Comments made in the podcast were inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA,” Bauchner said in the minute-long audio clip. “Racism and structural racism exist in the U.S. and in health care.”
RTWT
09 Jun 2018


Praxiteles, cast of torso of Aphrodite of Knidos by Ingres, Ecole des Beaux Arts, Paris.
And Feminists have a problem with that, reports Leah Kaminsky.
Take a tour of the female pelvis, and you’ll encounter a few incongruous people along the way. How did James Douglas end up tucked behind the uterus? What is Gabriel Fallopian doing hanging around the ovaries? Why is Caspar Bartholin the Younger attached to the labia? And can we trust Ernst Grafenberg’s claim that he actually found the G-spot? Whether you know it or not, each of these dudes have ended up immortalised in the female pelvis – as the Pouch of Douglas, Bartholin’s glands, fallopian tubes, and that elusive Grafenberg spot.
The truth is, men are all over women’s bodies – dead, white male anatomists, that is. Their names live on eponymously, immortalised like audacious explorers for conquering the geography of the female pelvis as if it were terra nullius. …
Gender bias in the teaching of anatomy and physiology to medical students was examined in a 2013 study by Susan Morgan and her colleagues. In textbooks used to instruct students, they found that “male anatomy and physiology are often represented as the norm, with women being underrepresented in nonâ€reproductive anatomy. The impression is gained that the human body is male and that the female body is presented only to show how it differs.â€
If many medical terms embody a patriarchal history, the question is how much it matters today. If most people don’t even realise that the names of female body parts have male origins – so don’t automatically connect them to men, rather than women – is it such a big deal? After all, for a word to bolster a sexist system, you’d think it would need to have some connection to male-oriented meaning in our minds.
One problem, says Lera Boroditsky, associate professor of cognitive science at UCSD, is that eponyms perpetuate the notion that advances are made by one individual – rather than the long collaborative process central to the process of scientific discovery. She argues for a system “that is not centred around the historical victories of men ‘discovering’ body partsâ€. Instead, these terms should be replaced by descriptors that are useful and educational to the body’s owner.
RTWT
07 Oct 2017

The Philadelphia medical dictionary: containing a concise explanation of all the terms used in medicine, surgery, pharmacy, botany, natural history, chemistry, and materia medica. 1817.
18 Mar 2017

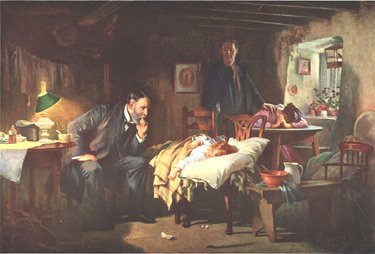
Sir Samuel Luke Fildes KCVO RA, The Doctor, 1891, Tate Gallery.
In 1949, Fildes’ painting “The Doctor” (1891) was used by the American Medical Association in a campaign against a proposal for nationalized medical care put forth by President Harry S. Truman. The image was used in posters and brochures along with the slogan, “Keep Politics Out of this Picture.” 65,000 posters of The Doctor were distributed, which helped to raise public skepticism of the nationalized health care campaign. In 2008, the AMA was no longer defending the sanctity of the doctor-patient relationship and the independence of the Medical Profession, but was instead supporting Obamacare and the nationalization of health care.
Dr. Publius, at Ricochet, explains how all this happened.
For the medical profession, there is one ethical obligation that surpasses all others. It is the very obligation that defines a classic profession, and once it is abandoned, members of that so-called profession no longer have any claim whatsoever to any of the special regard, respect, perquisites, or considerations that commonly accrue to true professionals in our society.
Physicians have referred to this obligation as the doctor-patient relationship. Like the lawyer-client relationship and the clergy-parishioner relationship, the doctor-patient relationship is supposed to be a sacred, protected, fiduciary one, in which the patient can feel safe in disclosing private information they may not even willingly tell their spouses, and in return the doctor agrees not only to keep that information private, but also to act on that information in such a way that furthers and optimizes the individual patient’s own best medical interests, without regard to which actions or recommendations might be to the doctor’s interests — or to society’s.
The abandonment of this sacred, fiduciary obligation (honored by physicians for over 2000 years) cannot be blamed on Obamacare. It was formally abandoned years before most of us had ever heard of Mr. Obama. The doctor-patient relationship, never as pure in practice as it was in concept, began to significantly erode in the 1990s. This, of course, was the heyday of for-profit HMOs, when the insurers used extreme coercion to make certain that doctors learned who their real customers were. Doctors who did not place the payers first had their reimbursements slashed, and often found themselves excluded from panels, and therefore from access to patients. In a surprisingly short time doctors by the thousands were signing “gag clauses,†in which they agreed to withhold from patients certain information that might be adverse to the interests of the HMOs.
It would be wrong to say that doctors did not mind these things. It troubled many of them deeply. Indeed, by the turn of the millennium many members of the profession were feeling, and occasionally publicly expressing, tremendous guilt for having had to abandon their chief ethical obligation to their patients, in order to continue practicing medicine.
Faced with an ethical dilemma which was increasingly difficult for them to tolerate, an outcry arose from within the medical profession demanding that their leadership take up the problem, and do something about it. Most doctors had in mind some sort of organized action by which the profession would attempt to reclaim its ethical grounding. And so, conferences were convened, debates (of a sort) engaged in, and at last, action taken.
What doctors in the trenches failed to realize was that the physicians who dedicate their careers to leading professional organizations are almost always Progressives, because this is what Progressives do. So the action that was finally taken was the official adoption of a new set of medical ethics, which was published in 2002: “Medical Professionalism in the New Millennium: A Physician Charter. “(Annals of Internal Medicine, February 5, 2002). This document described a new ethical precept which was to be formally adopted by the medical profession. That new precept was, of course, “Social Justice.†Under the precept of social justice, doctors, in making medical decisions at the bedside, suddenly became obligated to take the equitable distribution of healthcare resources into account. Covert rationing at the bedside at the behest of payers (who presumably knew more about equitable distribution of resources than individual physicians did), was not only acceptable, and not only a positive good, but an ethical requirement.
During the intervening years this new charter of medical ethics was indeed formally adopted by virtually every medical professional organization in the world.
Adding social justice to the ethical obligations of physicians or course did nothing to ease the discrepancy between the needs the patient and the needs of the payer. But its addition at least assuaged some of the guilt of some of the doctors who chose not to think too deeply about it.
This modernized, progressive version of medical ethics was not the result of Obamacare, but it has served Obamacare well. It was a matter of mere moments before doctors noticed that it would behoove them to shift their efforts from making the insurers happy to making the government happy.
Today, when a doctor makes a medical recommendation to a patient, that patient can no longer be confident that the recommendation is truly the one the doctor believes is best for him or her. For it may instead simply represent what the doctor has decided the patient deserves, given his/her needs in relation to the needs of all the other patients in the Accountable Care Organization, the state, the country, or the world.
21 Jan 2016


I grew up in Shenandoah, so I know McAdoo.
I came across a classic Coal Region survival story yesterday, out of McAdoo, just south of Hazleton.
WNEP:
Justin Smith, 26, of McAdoo is what doctors are calling a medical miracle.
He was found nearly frozen to death on the side of the road about one year ago.
On Monday, he got the opportunity to thank everyone who helped him survive after spending nearly 12 hours out in the cold.
“I got done with work that day and we were going to the fire hall to hang out, having a couple drinks with some people, and I wanted to go home around 10 o’clock,†said Smith.
On that cold night last February, Justin Smith walked out of the Treskow fire hall, but never made it home.
His father Don found him the next day on the side of Treskow Road.
“I looked over and there was Justin laying there and he was laying face up there like this,†said Don Smith. ” He was blue. His face he was lifeless. I checked for a pulse. I checked for a heartbeat. There was nothing.â€
“The coroner was on scene. The state police were on scene. They were doing essentially a death investigation,†said Dr. Gerald Coleman.
But Dr. Coleman, an emergency department physician at Lehigh Valley Hospital in Hazleton, refused to pronounce Justin dead when his body was that cold.
“Our mind is supposed to run the show, not our hearts because if your heart runs the show, you can run into some problems. I just kind of threw that to the wind and said, ‘No, not today,’†said Dr. Coleman.
A team in Hazleton performed CPR on Justin for two hours.
He was then transferred to Lehigh Valley Hospital Cedar Crest near Allentown where doctors used what’s called an ECMO machine to warm up Justin’s blood.
Doctors say flying Justin to Lehigh Valley’s Hospital near Allentown was a miracle in itself. They had to beat a snowstorm and do compressions on him the entire way.
“We knew we needed a big, big miracle,†Justin’s mom Sissy Smith said.
“When you have very low temperature, it can preserve the brain and other organ functions,†said Dr. James Wu of the Lehigh Valley Health Network.
Doctors said as Justin warmed up, his heart started beating.
Weeks went by before he actually woke up and realized where he was.
“It’s like I woke up from a dream, but it wasn’t a dream,†Justin said.
“When you look at the science of what happened to Justin, it was really hard to imagine that anyone on Earth could survive this,†said Dr. John Castaldo of the Lehigh Valley Health Network.
Now he’s back to his family he loves, golf, and school.
Justin lost his pinkies and all of his toes, but doctors call him a medical miracle.
31 Mar 2015

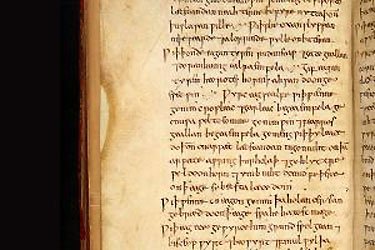
Bald’s Leechbook, British Library (Royal 12 D xvii)).
Scientists recently experimented with a recipe from Bald’s Leechbook aka Medicinale Anglicum an Old English medical text probably compiled in the ninth-century and found that a compound recommended for a common eye infection worked just as well as the modern antibiotic used to treat Methicillin-resistant Staphylococcus aureus (MRSA).
New Scientist:
The project was born when a microbiologist at the University of Nottingham, UK, got talking to an Anglo Saxon scholar. They decided to test a recipe from an Old English medical compendium called Bald’s Leechbook, housed in the British Library. …
Sourcing authentic ingredients was a major challenge, says Freya Harrison, the microbiologist. They had to hope for the best with the leeks and garlic because modern crop varieties are likely to be quite different to ancient ones – even those branded as heritage. For the wine they used an organic vintage from a historic English vineyard.
As “brass vessels” would be hard to sterilise – and expensive – they used glass bottles with squares of brass sheet immersed in the mixture. Bullocks gall was easy, though, as cow’s bile salts are sold as a supplement for people who have had their gall bladders removed.
After nine days of stewing, the potion had killed all the soil bacteria introduced by the leek and garlic. “It was self-sterilising,” says Harrison. “That was the first inkling that this crazy idea just might have some use.”
A side effect was that it made the lab smell of garlic. “It was not unpleasant,” says Harrison. “It’s all edible stuff. Everyone thought we were making lunch.”
The potion was tested on scraps of skin taken from mice infected with methicillin-resistant Staphylococcus aureus. This is an antibiotic-resistant version of the bacteria that causes styes, more commonly known as the hospital superbug MRSA. The potion killed 90 per cent of the bacteria. Vancomycin, the antibiotic generally used for MRSA, killed about the same proportion when it was added to the skin scraps. …
It wouldn’t be the first modern drug to be derived from ancient manuscripts – the widely used antimalarial drug artemisinin was discovered by scouring historical Chinese medical texts.
04 Oct 2014





hierarchical aestheticism: Goes mad and dies from a brain tumor; suffers more than a century of lies about it being due to syphilis.
———————————–
Telegraph:
Friedrich Nietzsche, the philosopher thought to have died of syphilis caught from prostitutes, was in fact the victim of a posthumous smear campaign by anti-Nazis, according to new research.
A study of medical records has found that, far from suffering a sexually-transmitted disease which drove him mad, Nietzsche almost certainly died of brain cancer.
The doctor who has carried out the study claims that the universally-accepted story of Nietzsche having caught syphilis from prostitutes was actually concocted after the Second World War by Wilhelm Lange-Eichbaum, an academic who was one of Nietzsche’s most vociferous critics. It was then adopted as fact by intellectuals who were keen to demolish the reputation of Nietzsche, whose idea of a “Superman” was used to underpin Nazism.
The new research was carried out by Dr Leonard Sax, the director of the Montgomery Centre for Research in Child Development in Maryland, America. Dr Sax made his discovery after studying accounts of Nietzsche’s collapse with dementia in 1889.
Full article.
18 Jul 2014


Carl Zimmerman‘s article at Ars Technica offers a useful precis.
Why do 40 percent of Caucasians have Type A, while only 27 percent of Asians do? Where do different blood types come from, and what do they do?
To get some answers, I went to the experts—to hematologists, geneticists, evolutionary biologists, virologists, and nutrition scientists. In 1900, the Austrian physician Karl Landsteiner first discovered blood types, winning the Nobel Prize for his research in 1930. Since then, scientists have developed ever more powerful tools for probing the biology of blood types. They’ve found some intriguing clues about blood types—tracing their deep ancestry, for example, and detecting influences of blood types on our health. And yet I found that in many ways, blood types remain strangely mysterious. Scientists have yet to come up with a good explanation for their very existence.
“Isn’t it amazing?†says Ajit Varki, a biologist at the University of California at San Diego, “Almost a hundred years after the Nobel Prize was awarded for this discovery, we still don’t know exactly what they’re for.”
I’m Type O, RH positive myself.
23 Aug 2012


Klebsiella pneumoniae
The New York Times has a scary and intriguing medical detective story.
The ambulance sped up to the red brick federal research hospital on June 13, 2011, and paramedics rushed a gravely ill 43-year-old woman straight to intensive care. She had a rare lung disease and was gasping for breath. And, just hours before, the hospital learned she had been infected with a deadly strain of bacteria resistant to nearly all antibiotics.
The hospital employed the most stringent and severe form of isolation, but soon the bacterium, Klebsiella pneumoniae, was spreading through the hospital. Seventeen patients got it, and six of them died. Had they been infected by the woman? And, if so, how did the bacteria escape strict controls in one of the nation’s most sophisticated hospitals, the Clinical Center of the National Institutes of Health in Bethesda, Md.?
What followed was a medical detective story that involved the rare use of rapid genetic sequencing to map the entire genome of a bacterium as it spread and to use that information to detect its origins and trace its route.
Read the whole thing.
Hat tip to Stephen Frankel.
26 Jun 2012
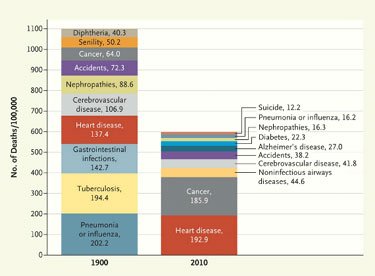
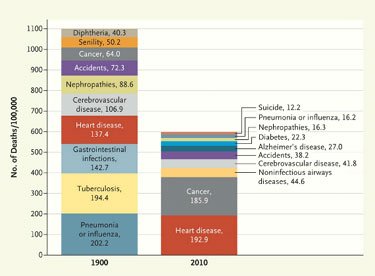
Celebrating its 200th anniversary, the New England Journal of Medicine takes a look back, comparing causes of death in 1811, 1900, and 2010.
We have more heart disease and cancer, and seem to less frequently expire due to spontaneous combustion or the impact of a cannon ball. Fears of racial suicide and belief in the progress of eugenics are not what they were in 1912.
Hat tip to Sarah Kliff.
08 May 2012


Robert Liston
Atul Gawande shares a great story of the pre-anaesthesia age, in the New England Journal of Medicine.
The limits of patients’ tolerance for pain forced surgeons to choose slashing speed over precision. With either the flap method or the circular method, amputation could be accomplished in less than a minute, though the subsequent ligation of the severed blood vessels and suturing of the muscle and skin over the stump sometimes required 20 or 30 minutes when performed by less experienced surgeons. No matter how swiftly the amputation was performed, however, the suffering that patients experienced was terrible. …
Before anesthesia, the sounds of patients thrashing and screaming filled operating rooms. So, from the first use of surgical anesthesia, observers were struck by the stillness and silence. In London, [Robert] Liston called ether anesthesia a “Yankee dodge†— having seen fads such as hypnotism come and go — but he tried it nonetheless, performing the first amputation with the use of anesthesia, in a 36-year-old butler with a septic knee, 2 months after the publication of Bigelow’s report. As the historian Richard Hollingham recounts, from the case records, a rubber tube was connected to a flask of ether gas, and the patient was told to breathe through it for 2 or 3 minutes. He became motionless and quiet. Throughout the procedure, he did not make a sound or even grimace. “When are you going to begin?†asked the patient a few moments later. He had felt nothing. “This Yankee dodge beats mesmerism hollow,†Liston exclaimed.
It would take a little while for surgeons to discover that the use of anesthesia allowed them time to be meticulous. Despite the advantages of anesthesia, Liston, like many other surgeons, proceeded in his usual lightning-quick and bloody way. Spectators in the operating-theater gallery would still get out their pocket watches to time him. The butler’s operation, for instance, took an astonishing 25 seconds from incision to wound closure. (Liston operated so fast that he once accidentally amputated an assistant’s fingers along with a patient’s leg, according to Hollingham. The patient and the assistant both died of sepsis, and a spectator reportedly died of shock, resulting in the only known procedure with a 300% mortality.
In his surgical exuberance, Liston apparently had cut through the coat tails of a distinguished visitor, who thought he’d been stabbed in the vitals and proceeded to die of fright.
14 Mar 2012
Run Google image searches on: “Penile Fracture” and “Peyronie’s disease.” I’m not posting pictures.
————————-
Jeff Winkler had a rather unusual, and incredibly unpleasant to even contemplate, accident.
With my one kidney, the Meckel’s diverticulum was unable to dissipate a blood clot causing aortic arrhythmia, which led to the ruptured penile corpus fracture and Peyronie’s disease. It was a freak accident.
/div>

Feeds
|